Who might be a relevant client for Jesse?
What kinds of therapy does Jesse practice and what might it be like?
Where and when can therapy take place?
How to access therapy (referrals & fees)?
Who might be a relevant client for Jesse?
“There is one proper diagnosis: the human condition (and I’m pretty sure a lot of other animals deal with something similar)”.
Jesse works with adolescents (15 years+) and adults at all levels of wellness and functioning: those who have required hospitalisation due to their mental health and experienced living as unbearable, to those who are ‘doing-well’ yet experience a lack of fulfilment or ‘well-being’ in life. He believes that mental health is unfairly supported when compared to physical health. For some, therapy is critical healthcare (like surgery or rehabilitation). For others, therapy is health development (like personal training). For most, it’s somewhere in-between. For anyone, it can be worthwhile.
Special interests are listed below but some of Jesse’s expertise is particularly put towards helping people who describe some of these issues:
- ‘Workaholism’, perfectionistism, and struggling with tolerating uncertainty.
- Not being able to ‘shut off’ and/or being overly confused by their mind.
- Being disconnected from and/or overwhelmed by their body and emotions (including medical symptoms that seem to stem from these difficulties).
- ‘People pleasing’ and struggling with boundaries.
- Feelings of guilt, inadequacy, and/or ‘imposter syndrome’ (including a lack of sense of identity/’pretending’ rather than simply being their self).
- Difficulty trusting and relying on their self or others (e.g., over-reliant upon or avoidant of support, closeness, and care from others).
- Being stuck in patterns of behaviour even that they ‘know’ are unhelpful.

Special Interests
Trauma
Personality conditions
Dissociative conditions
Functional neurological/bodily conditions
Treatment-resistant conditions (e.g., depression/anxiety)
Existential fulfilment

Veterans and
First Responders
Jesse has extensive experience in working with those with trauma from defence and first-responder roles. He believes that trauma for such people often goes beyond shocking events witnessed and experienced in their role. Jesse ensures space for acknowledging and working with this side of service-related trauma:
Social alienation: Feeling out-of-place from civilian life and society as well as out-of-place from the service community following leave or discharge.
‘Collateral trauma’ guilt: Witnessing and feeling guilt and shame for impacts of personal trauma on family and close-ones.
Identity grief: Experiencing a sudden and profound loss of self-identity and purpose through the loss of the service role.
Betrayal and moral injury: Feeling betrayed through a lack of care and support from the institution served. The “protect and serve” morals of service personnel feel violated with experiences of “neglect and desert” by those that they have served (often worsened by undergoing DVA and insurance processes). Or a sense of having failed to protect and serve where the role involved harming others (e.g., combat or use of physical intervention) or situations where others could not be helped (e.g., ‘failed’ missions or jobs).

First Nations People
Jesse’s clinical training involved working in an Aboriginal mental health service under mentorship of Aboriginal clinicians. He was also co-secretary of the initial working party for improving cultural safety and First Nations-informed education the University of Newcastle. He brings the learned cultural wisdom of these experiences to all clients, but especially those of First Nations identities.
What kinds of therapy does Jesse practice and what might it be like?
Kinds Of Therapy
Jesse primarily uses contemporary psychodynamic and trauma-focused treatments, particularly MBT (Mentalization-Based Treatment), CM (Conversational Model and its short forms, PIT & STIDP; Psychodynamic Interpersonal Therapy & Short-Term Dynamic Interpersonal Dynamic Psychotherapy), and EMDR (Eye-Movement Desensitisation Reprocessing) therapy.
He also has some formal training in and makes relevant use of Aboriginal Culturally-Informed Counselling, CBT (Cognitive Behavioural Therapy), CBT-E (Enhanced/for Eating-Disorders), IR (Imagery Rescripting for Childhood Trauma), ISTDP (Intensive Short-Term Dynamic Psychotherapy), FPT-ED (Focal Psychodynamic Therapy for Eating Disorders), IPT (Interpersonal Psychotherapy), MI (Motivational Interviewing), DBT (Dialectical Behaviour Therapy), (Radically Open) RO-DBT, suicide prevention and management, and Vipassana mindfulness training.
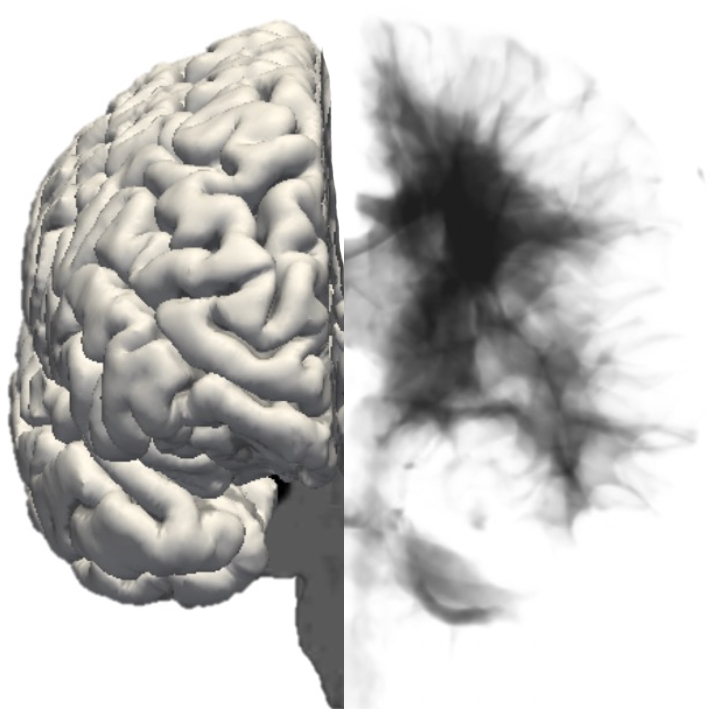
Jesse’s primary theoretical basis is in active inference – a theory of mind, brain, and behaviour that is based in neuroscience, physics, and probability theory, and gives a unifying explanation of life itself. He believes that it can bring different therapy models (which have different theoretical perspectives) under the same umbrella and guide which practical parts of them are more or less useful for different people at different times.
What Therapy Might Be Like
“When it comes to improving our mental health, no-one else can do it for us, but we can’t do it without someone else”.
Therapy will generally be conversational rather than educational. Rather than teach you skills and knowledge Jesse will primarily use his expertise to explore and discover ‘you’ with you, to then practice change for ‘you’ with you*. Less than being focused on symptom-management he will be interested in discovering what underlies and keeps symptoms going (i.e., “the roots of problems”) to not just “treat illness” but facilitate wellness and growth. Problems and patterns from your outside life will be raised in the therapy, to then explore, work through and create change together in the therapy; which will then be raised and be worked though in your everyday life. Again, this will be done with you (not ‘to you’ or ‘for you’), through a therapeutic relationship of curiosity, trust, compassion, genuineness, and (attempted) good humour.
Note* this approach is often challenging for people who are perfectionistic, overly ‘results-driven’, and struggle with uncertainty in life; and an intentional part of practicing change for where these are part of the problem.
Where and when can therapy take place?
Following a recent relocation – Jesse is currently only available via Telehealth.
Telehealth: 8am – 4pm (AWST) Mondays & Fridays
Fixed Schedule Arrangement
Jesse works from a fixed therapy schedule. This means that you will be allocated a fixed session time each week. Although this unfortunately means less flexibility of scheduling, it means better consistency, predictability, and availability for your sessions. Frequency of sessions can be decreased (fortnightly/monthly) as becomes relevant, however frequency increases depend upon availability from other clients reducing or completing therapy. The fixed session is expected to be prioritised over other appointments and work commitments and cancelled only where attendance is not possible in-person or via Telehealth (holidays etc. with sufficient notice are exempted). The fixed session time is a mutual commitment and it is important to consider if this approach is suited to you.
How to access therapy (referrals & fees)?
The APS National Schedule of Recommended Fees 2025-2026 has the standard 46 to 60-minute consultation fee set at $318 for psychology services (this does not specify rates to those with an area of endorsement; an approx. 38% difference under Medicare).
To try to keep therapy financially feasible, the standard fee is $220 per 50min session for those paying out-of-pocket. Report writing is charged pro-rata to this. This is unfortunately still financially challenging for many, and various fee supports are needed:
Medicare – Current Medicare rebates for clinical psychology are $145.25 for 10 sessions per calendar year. This means that the payable out-of-pocket gap is $74.75 per session for 10 sessions but the full amount ($220) thereafter.
Under Medicare, GP appointments are required for the initial referral and after 6 sessions (for approval of 4 further sessions).
For qualifying eating disorders, up to 40 sessions per calendar year are available. GP appointments are required for the initial referral and after the 10th, 20th, and 30th session. A psychiatrist review is required at 20 sessions.
Private Health – Most private health funds provide reimbursement for clinical psychology under certain levels of ancillary coverage. Generally the amount covered and number of sessions covered is less than Medicare. Please consult your fund for personalised information. A GP referral is sometimes required for accessing therapy under private health.
NDIS (Self-Managed) – Those under self-managed funds may have approval for clinical psychology, with the standard NDIS rate payable. Jesse is not NDIS registered to provide under plan-managed cases. A GP referral is required for accessing therapy under NDIS.
DVA – The department of veterans affairs offers funding options (under white card and gold card) for clinical psychology, with fees stipulated by the federal government. Gap fees are not chargeable for these services. Cancellation fees are not covered by DVA and are payable by the client. Treatment is provided in ‘cycles’ of 12 sessions, with GP referral required for each new cycle (though a GP can approve referrals to be valid for 3, 6, or 12 months periods rather than 12 sessions when relevant).
WorkCover – Insurers provide funding options for clinical psychology under workers compensation, with fees stipulated by the state government. Gap fees are not chargeable for these services. Cancellation fees are not covered by insurers and are payable by the client. A GP referral and insurer approval are required for accessing therapy under WorkCover.
Cancellation Fees
A minimum of two business days notice is required for cancelling an appointment. Although Jesse works from a fixed-schedule, clients will sometimes be wanting another session in the week and appropriate notice allows the time to be filled. Where sufficient notice is not given or cancellation occurs due to prioritisation of work or other appointments and the session cannot be filled, a fee of $110 applies (this is not covered by Medicare, private health funds, DVA, or WorkCover).